Proponents of health care simulation education have said for years that it improves clinician performance and reduces patient safety errors, but until recently they have lacked the data and evidence to share with academic leaders and policymakers.
Simulation education in health care has advanced rapidly in the past decade, due in large part to the efforts of nurse educators. The National Council of State Boards of Nursing (NCSBN) in 2014 released the results of a landmark simulation study, which was followed up in 2015 by the publication of the National League for Nursing (NLN) Jeffries Simulation Theory. GW Nursing Dean Pamela Jeffries’ work as one of the consultants of the NCSBN study and her eponymous theory helped legitimize simulation education in pre-licensure nursing education.
The NCSBN National Simulation Study examined the role and outcomes of simulation in pre-licensure nursing education. The study provided substantial evidence that simulation can be effectively substituted for up to 50 percent of traditional clinical experience in all pre-licensure nursing courses, under conditions comparable to high-quality, high-fidelity situations described in the study.
The study results reaffirmed simulation education advocates’ belief in this type of experiential learning strategy while providing concrete data to address concerns held by simulation skeptics. The research team had its own skeptics—they were unsure of how well simulation could supplement traditional clinical experiences in certain areas, including mental health, pediatrics and obstetrics, but the data showed no significant differences as long as the correct simulation technique was used.
“For me personally, it was those areas that the simulation worked for that surprised me a little, as someone who likes traditional clinical experiences,” said Nancy Spector, the NCSBN director of regulatory innovations and a consultant on the study.
Study results influence state policy
The NCSBN study marked a shift in how nursing schools and policymakers viewed simulation education. Each state’s board of nursing makes its own decisions regarding how much simulation can be used to supplement traditional clinical experiences in pre-licensure programs. After the NCSBN study was published, many states amended their policies and increased the amount of allowable simulation. “The study has had a really positive impact on what boards of nursing are allowing,” Dr. Spector said. There was no evidence before the study, so boards made arbitrary decisions regarding simulation, and some states didn’t allow any amount of simulation to be used to supplement clinical experiences.
One year after the study was published, the NCSBN convened an expert panel to develop national simulation guidelines for pre-licensure nursing programs. These guidelines included evidence to support the use of simulation and information for faculty and program directors on how to incorporate high-quality, high-fidelity simulation in their programs.
Since the NCSBN released these guidelines in 2015, more than half of all pre-licensure programs in the country have adopted them, according to a survey conducted by the NCSBN evaluating the simulation landscape. That survey also revealed that high-fidelity simulation use has substantially increased for almost all undergraduate courses since 2010.
High-quality simulation fosters better student outcomes
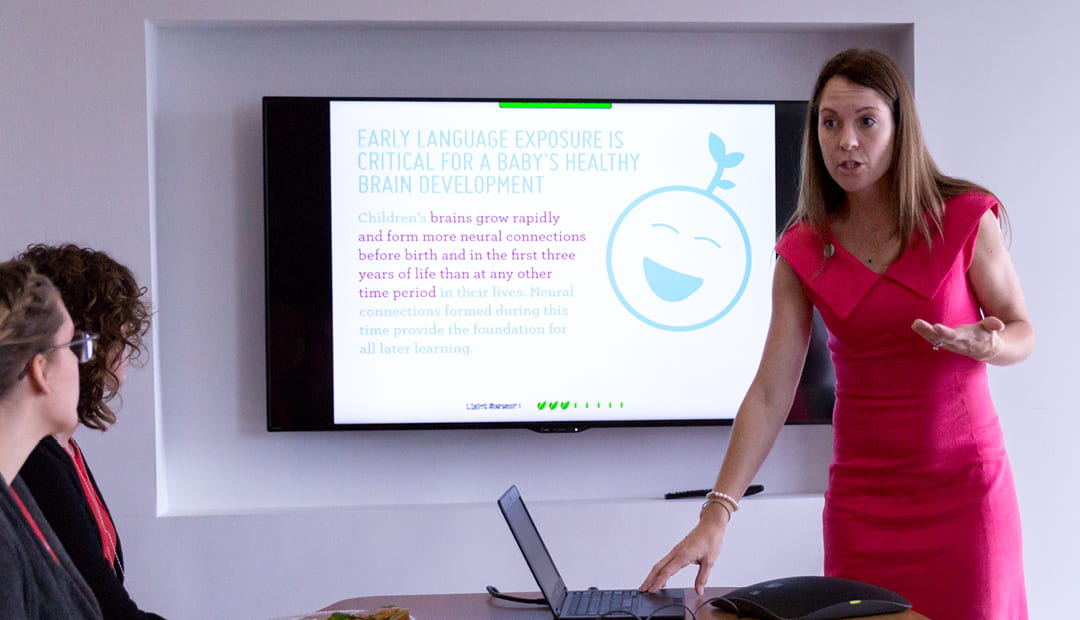
GW Nursing is committed to providing students with high-quality, high-fidelity experiences and has made significant investments in simulation under the direction of Dr. Jeffries, an innovator in promoting and advancing the field of simulation education.
Recent renovations at Innovation Hall on GW’s Virginia Science and Technology Campus nearly doubled the simulation space available to nursing students. The new Objective Structured Clinical Examination (OSCE) center contains 12 patient exam rooms and two acute care rooms, bringing the total simulation space available to both undergraduate and graduate students to nearly 20,000 square feet.
While the new OSCE space was designed for nurse practitioner students to improve their clinical skills, GW Nursing also recently invested $400,000 in upgrades to make simulation as comparable to a hospital setting as possible for undergraduate students, said Crystel Farina, the school’s director of simulation and experiential learning. Those upgrades include eight new moderate-fidelity simulators (manikins that breathe and have a pulse to practice certain skills, but with fewer features than high-fidelity manikins), new beds, IV pumps, medication dispensing machines and workstations on wheels. The school launched another renovation this spring that will add additional simulation and debriefing space, new technology, a virtual reality space and a simulated operating room.
As simulation director, Ms. Farina ensures that all of the school’s many simulation events run smoothly. Simulation is integrated throughout GW Nursing’s entire curriculum—every course has some sort of simulation experience in it, Ms. Farina said. “My role is to ensure that not only does the simulation continue, but that it’s high quality and meets the standards of best practice,” she said.
Those standards, which are set by the International Nursing Association for Clinical Simulation and Learning (INACSL), were developed based on the NLN Jeffries Theory and the NCSBN guidelines. Nursing schools now have a solid framework and explicit standards to guide the development of high-quality simulation experiences. While the virtues of simulation as a teaching strategy are well established, Ms. Farina and other dedicated simulation educators are quick to point out that it’s crucial that students engage in high-quality, high-fidelity simulations. When simulations are conducted improperly, or not in accordance with the guidelines and standards set forth by NCSBN and INACSL, simulation can actually be harmful to students.
In the early days of simulation use, instructors would purposefully introduce mistakes into a simulation in the hopes that students would catch the mistake, Ms. Farina said. “We didn’t know how important it was to the students’ self-esteem and to their socialization as a nurse if they didn’t catch the mistake,” she explains.
The NLN Jeffries Theory set forth guidelines that simulation should be collaborative and transparent—the student, simulated patient (if one is used) and faculty should know exactly what’s expected and what the objectives are.
“There’s no way students can meet the objective if they get caught up in how to program the IV pump,” Ms. Farina said.
Schools that implement high-quality and high-fidelity simulation have seen improvements in student performance and clinical confidence. “Anecdotally, we’re seeing much better outcomes from simulation now that we have the NLN Jeffries Theory,” Ms. Farina said. “Their ability to talk with each other and other care providers is definitely enhanced. Their teamwork is also much better—they’re able to work as a team, and they don’t see things as individual tasks.”
Dr. Jeffries’ groundbreaking work has influenced nurse educators for years, even before the publication of the NCSBN study and her eponymous theory. Jeffries’ 2007 book, “Simulation in Nursing Education”, was Kellie Bryant’s go-to resource when she was hired as the director of simulation learning at New York University College of Nursing in 2008.
“From my experience, her book was how a lot of us got started in simulation,” Dr. Bryant said. “I’m talking over 10 years ago when there weren’t conferences or other books or journals—that book was our template for simulation.”
In her current role as executive director of simulation at Columbia School of Nursing, Dr. Bryant is using Dr. Jeffries’ evidence-based approach to developing high-quality simulations, with a focus on creating simulation experiences that address proper medication administration. “We know that medical errors are a leading cause of mortality and death, and a component of that is giving the wrong medication or the wrong dose,” she explained.
Dr. Bryant and her colleagues began with manikin-based simulations, then moved on to using standardized patients (actors portraying patients) for students to practice the proper protocols, such as reading a patient’s chart correctly, conducting safety checks, scanning a patient’s identification band and more. “The clinical instructors in the hospital are reporting that students have stronger skills than in the past, and seem more comfortable with medication administration,” Dr. Bryant said. “That’s because of simulation, because of deliberate practice. Students understand the rationale, and realize for each step why it’s important to follow protocol.”
Best practices and certifications for simulation educators
Although Dr. Bryant relied heavily on Dr. Jeffries’ early books for guidance due to the lack of available training opportunities, she cautioned novice educators against jumping into simulation.
“All schools are realizing that if they don’t have a simulation program or a simulation-based curriculum, then they’re behind the curve,” she said. “Everyone knows they have to use simulation, but people aren’t really prepared to utilize it the best way. You have to be trained, you have to have that theoretical background and you need to know what you’re doing.”
For aspiring simulation educators, that begins with securing support from their school’s leadership as well as procuring funds to attend a training program or conference. “Education is the key—before you can start using it with students and teaching other faculty, you have to know what you’re doing and have that expertise first to utilize it and to teach others,” Dr. Bryant said.
Without simulation training and instruction on what qualifies as high quality and high fidelity, schools will be out of compliance with the NCSBN and INACSL standards.
Educators who are committed to advancing their simulation knowledge and skills can become professionally certified. The Society for Simulation in Healthcare developed its Certified Healthcare Simulation Educator (CHSE) certificate in 2012 to recognize educators for their expertise in simulation. The certification demonstrates that an individual is committed to simulation and has specialized skills and knowledge.
Nursing schools with CHSE-certified educators ensure that their simulation is high quality and high fidelity, which is key to following the standards and best practices set forth by the NCSBN simulation study and the subsequent guidelines.
“If you have a CHSE-certified person in your simulation center, you have high quality and high fidelity,” Ms. Farina said. “It really does support what the study was requiring. A lot of schools out there are doing simulations but are completely missing that high-quality, high-fidelity piece because they don’t know the pedagogy.”
Interprofessional simulation
While nurse educators have advanced the field of simulation and set the standards for assessing clinical skills, other health care professions have also been using simulation technology for years.
Chad Epps, executive director at the Center for Healthcare Improvement and Patient Simulation at the University of Tennessee Health Science Center, recalls using a simulation-based model for practicing anesthesia during his medical residency program in 2001. “I learned how to use anesthesia on a simulator before I ever did it on a patient,” he said. “That left an impression on me in terms of its potential as an educational modality.”
Dr. Epps pursued his interest in education and simulation as he embarked on a career as an anesthesiologist. He became the director of simulation at the University of Alabama at Birmingham (UAB), where he started a program for nurse anesthetists and developed the curriculum, which included interprofessional simulation experiences. In his various simulation educator positions, Dr. Epps has pushed for more interprofessional experiences that mimic real-world clinical environments.
“We graduate these professional health students, and they go into clinics and the clinical world, and they’re suddenly exposed to all of these other professions,” he explained. “In the past, [these students] never learned anything about those professions so they didn’t know what their role was, or what the other professions’ role was.”
During his time at UAB, Dr. Epps and his colleagues developed simulation experiences for nursing and medical students that included specific competencies developed by the Interprofessional Educational Collaborative with intentional objectives related to the Team Strategies & Tools to Enhance Performance & Patient Safety (TeamSTEPPS) teamwork system for health care professionals designed by the Agency for Healthcare Research and Quality. Studies have shown that hospitals that implement TeamSTEPPS have improved patient outcomes, and Dr. Epps wanted the medical and nursing students to become familiar with that model of communication.
“At first, students thought [the interprofessional simulation] felt very strange,” he said. “But it got to the point where if we did a simulation with just medical students and the nursing students weren’t there, they’d look around and say, ‘Where are the nursing students, something’s wrong.’”
In addition to increasing interprofessional experiences among health care students, Dr. Epps said he expects to see simulation used more widely among health care providers to improve patient safety. “We shouldn’t just use simulation for students, we should use simulation for practicing professionals,” he said. “The airline industry has done this—if you’re a commercial pilot, you have to go through simulation every six months or you risk losing your license. We don’t have that in health care yet, although we probably need it.”
Where does simulation go from here?
Simulation-based curricula and the use of simulation have been adopted by the majority of pre-licensure nursing programs. Our work continues in conducting the research to design best practices and to learn more about how simulation-based experiences affect student learning and, ultimately, patient outcomes and quality, safe care.
AUTHOR meredith lidard kleeman