Improving nurse education
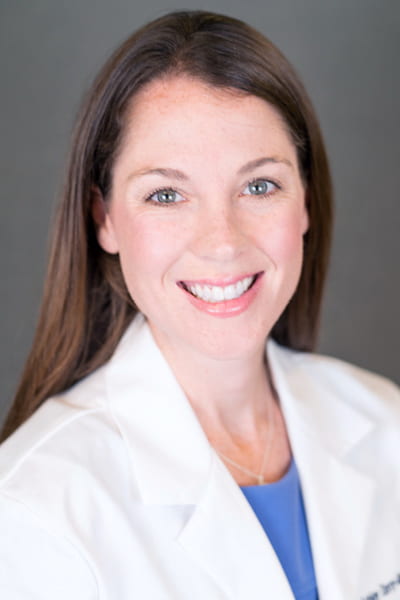
When Sarah Beebe began the Ph.D. program at GW Nursing, she made it a priority to complete her degree in three years. Despite the onset of a global pandemic that continues to upend daily routines and well-laid plans, Ms. Beebe is on track to defend her dissertation and graduate in spring 2022.
“I never missed a beat,” she proudly states, “but I might have missed a lot of sleep.”
Prior to joining the School of Nursing’s inaugural Ph.D. cohort in 2019, Ms. Beebe spent eight years working as a women’s health nurse practitioner and certified nurse-midwife in Delaware and Pennsylvania. She spent three of those years as a nurse and five as a midwife/nurse practitioner. In 2017, she became a full-time faculty member at the University of Delaware School of Nursing, teaching an undergraduate women’s health course.

“One of the reasons I love simulation is that we can practice different skills and reduce the risk of errors.”
– Sarah Beebe
After conducting some small independent research studies, Ms. Beebe recognized that she needed formal training and education to advance her understanding of research science. “I saw research as a puzzle, and I wanted to be better at putting that puzzle together,” she explains.
During her time at the University of Delaware, Ms. Beebe became a certified health care simulation educator, and that interest in simulation led her to apply for GW’s Ph.D. program.
Ms. Beebe’s dissertation investigates metacognition in family nurse practitioner students to understand the link between diagnostic reasoning and diagnostic errors, using simulation. “Diagnostic error is a major [patient safety] concern,” she says. “One of the reasons I love simulation is that we can practice different skills and reduce the risk of errors.”
Ms. Beebe left her full-time faculty position to commit to earning her Ph.D. as quickly as possible. That commitment was made possible in part by the McNelis Nursing Education Research Dissertation Award. “Dr. McNelis really values nursing education research,” Ms. Beebe notes. “We see educational research as improving future nurses and providers so that they can make new strides in clinical research and practice.”
Ms. Beebe plans to return to academia after completing the Ph.D. program. “But this time I’ll know what I’m doing,” she adds.
Treating the whole patient
Chad Huckabee plans to take to the skies. As a life flight nurse that is. He knows he will achieve his lofty goals, just as he knows what grade point average he will achieve upon graduation (somewhere between 3.7 and 4.0). Mr. Huckabee sets high standards for himself, thanks in part to his 10 years in the U.S. Marine Corps.

“Being a physical therapist didn’t match up with my thoughts of patient care. It was more about treating symptoms than taking care of the person holistically, which is what I wanted to do.”
– Chad Huckabee
Mr. Huckabee was drawn to a career in nursing after stints as a police officer and time spent studying to become a physical therapist in Texas. “Being a physical therapist didn’t match up with my thoughts of patient care,” he says. “It was more about treating symptoms than taking care of the person holistically, which is what I wanted to do.”
Eager to complete a new degree and begin his nursing career, Mr. Huckabee researched accelerated B.S.N. programs and ultimately chose GW. “What brought me to GW was the veteran compatibility,” he explains. “Most of my professors are veterans; having that to lean on [was important]. And they’re well ranked in the United States. If I was going to learn to be a nurse, I wanted to learn to be a nurse from a program that has high standards.”
Mr. Huckabee used his GI Bill to fund his PT degrees, leaving him to pay for his nursing degree on his own, but he received help from the GW Hospital Women’s Board Scholarship. “The scholarship put a dent in the student loans I have to pay back when I graduate—it’s a financial lift for me and my family,” he says.
That financial support helps Mr. Huckabee focus on his first weeks of clinical rotations in the medical surgical unit of GW Hospital. “It was what they said it was—hard, fast, crazy, but fun,” he says. “But for me, I thrive in chaos and disorder. My first day, I was taken aback by how different each patient could be, but what I learned and experienced I was able to start putting together.”
Mr. Huckabee is energized by the challenge of treating patients and he looks beyond traditional categories that might define them. “It’s about looking at the patient holistically, not just what they came to the hospital for,” he notes. “I want to take care of the patient and give them a full therapeutic idea of how they can help themselves, rather than treating symptoms and diagnoses.”
A passion for serving others
Moses Win has faced life-threatening challenges since the day he was born. His family belongs to the Karen people of Burma (now known as Myanmar), an ethnic minority that has been persecuted by the Burmese military for decades. Mr. Win was born and raised in the delta division of Burma and later escaped to a refugee camp in Thailand. His childhood was filled with obstacles—he received little education and suffered from bouts of illness because of the camp’s poor living conditions.
The nurses who cared for him in the refugee hospital made a lasting impression. “Fortunately I survived, but many young kids like me did not,” he says. “I thank God for my miracle, that I am still here, and for all the nurses who nursed me back to health.”

“I’m more motivated than ever to become a nurse to help others and provide for my family.”
– Moses Win
Mr. Win immigrated to America as a teenager with the help of the U.N. Refugee Agency and Catholic Charities. “[Catholic Charities] took care of me while I came here as a teenager alone,” he recalls. “I didn’t know anybody, I didn’t speak English.” He wanted to join the military “and pay back this country by serving, because they took me in,” he explains.
His first attempt was denied because he didn’t have a high school diploma. He pursued a high school diploma while working full-time and mastering English. His second attempt to join up was also denied because his online diploma was missing certain credits. Mr. Win enrolled in Houston Community College to receive additional credits while working part-time. The third time was the charm, and he joined the U.S. Navy in 2011 because “I would get to experience the world, and maybe be able to visit Thailand or Burma,” he says.
During his time in the Navy, Mr. Win received a medical technology associate’s degree from GWU. He went on to become an officer in the Navy Medical Service Corps and worked as a health care administrator, but it didn’t feel like his calling. His positive experience at GWU led him to the GW School of Nursing, where he received the William and Joanne Conway Transitioning Warrior Nursing Scholarship, which covers 50 percent of an incoming veteran’s tuition.
The scholarship supports Mr. Win’s immediate and future nursing goals, which include returning to hospitals along the Thai-Burmese border. “Burma’s current situation is very volatile, and my parents and sisters are in distress,” he explains. “I’m more motivated than ever to become a nurse to help others and provide for my family.”
AUTHOR Meredith Lidard Kleeman