The GW School of Nursing’s Center for Aging, Health and Humanities (CAHH) is on a mission: to make the world more age-friendly and livable for people throughout their span of life, by cultivating partnerships and generating innovative ideas.
The term “age-friendly” was first used by the World Health Organization in 2002 and was part of a strategy to improve the inclusion of older adults in cities and communitiesi. The age-friendly movement seeks to improve the economic, physical, and social environments through the “8 domains of livability”: housing; outdoor spaces and buildings; transportation; communication and information; civic participation and employment; respect and inclusion; health services and community supports; and social participationii.
Melissa Batchelor, Ph.D., RN-BC, FNP-BC, FGSA, FAAN, director of the CAHH, said that “age-friendly initiatives work to reduce the impact of ageism in society.” Ageism is “largely absent from the national dialogue on equity and inclusion,” she said, but it can “accelerate negative health outcomes for people,” especially at the intersection of racism and sexism. Dr. Batchelor said it is therefore a “national imperative to start and amplify the conversation about becoming more age-friendly.”

Additionally, creating an age-friendly world should be of interest to people of all ages because “what we do now to make our communities good places to grow up and grow old will yield returns not only for today’s elders but also tomorrow’s—that is, for all of us.”iii After all, there’s one thing about aging— “everyone’s doing it.”
The CAHH has been involved with age-friendly initiatives since 2019 when it co-hosted, with the Center for Health Policy and Media Engagement, a seminar featuring Dr. Terry Fulmer, in which she discussed the Age-Friendly Health Systems initiative.
Since 2019, the CAHH has received three consecutive years of University Seminar Series grant funding, allowing it to host multiple age-friendly talks focused on four core areas: age-friendly businesses, health systems, arts and creativity, and long-term care workforce.
On May 4 and 5, 2021, the CAHH hosted the inaugural Age-Friendly Ecosystem Summit in conjunction with its Age-Friendly regional municipality partners: Age-Friendly Alexandria, Arlington, D.C., City of Hyattsville, and Montgomery County. This summit was the first of its kind: a convening of age-friendly regional leaders designed to raise awareness of national age-friendly initiatives, inspire cross-collaboration, and learn about best practices from each of these age-friendly partners and regional thought leaders.
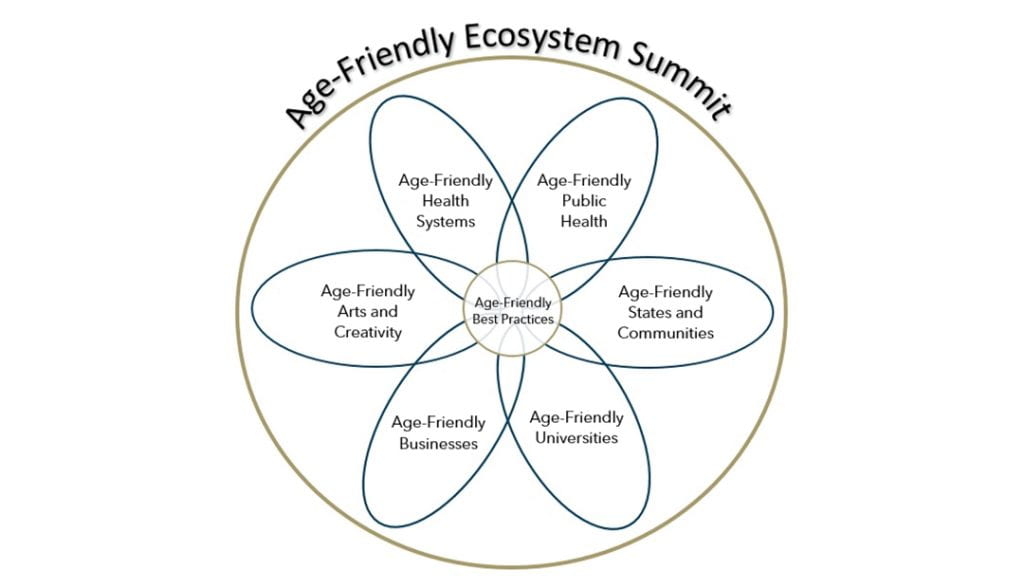
On day one, regional leaders presented LIVE “TED Talks” to share best practices, frameworks, and resources to advance an age-friendly ecosystem. On day two, local municipal leaders shared best practices and exemplary case studies of age-friendly initiatives. The group’s efforts were guided by a Venn diagram that depicts how various societal sectors are distinct while also connected, and are equally important in creating a wholly age-friendly society.
All of the money raised from this event helped to fund the Gene Cohen Research Award. Named after the CAHH’s founder and a pioneer in creative aging, this new scholarship is intended to support GW students to conduct interprofessional research on the impact of the arts and humanities on the health and well-being of older adults and persons with dementia.
Interested in the work of this summit or in supporting the Gene Cohen Research Award? Click the link below to purchase the recorded summit.
The summit and this type of collaboration is important, especially in an interconnected region like the greater Washington, D.C., area. It provided an opportunity for the age-friendly municipalities to step out of their silos, share best practices, expand partnerships, and replicate good ideas. “This type of sharing, replication, and lending of expertise only improves the lives of all residents in this region—and serves as a national model for the power of collective age-friendly initiatives,” said Dr. Batchelor. The hope is for this summit model to be replicated in other regions and to see more age-friendly communities created and strengthened.
When asked about the way in which the partnership between GW and the age-friendly municipalities has made a difference, Marci LeFevre, one of the CAHH’s partners and the age-friendly program lead for the City of Hyattsville, Maryland, said:
“By partnering with one another, we’re accelerating the discovery and exploration of promising policies, programs, and practices implemented by age-friendly programs elsewhere that can be replicated in our own municipalities. This is invaluable as the DMV region has a wealth of age-friendly resources, but they’re not necessarily widely known or promoted within and beyond our respective jurisdictions… By spotlighting and seeking ways to address these trends, such as the growing number of older adults experiencing homelessness in the DMV region, we can help identify and foster needed systems-level changes within and beyond our municipalities.”
As an extension of the age-friendly efforts of the Ecosystem Summit, the CAHH was a recipient of the AARP Community Challenge Grant in 2021.
The grant was used to support the CAHH’s event on October 27, 2021, the Age-Friendly Social Innovation Challenge. This event brought together a diverse, intergenerational group—including students, older adults, and working professionals—to design innovative strategies for building age-friendly infrastructures. The CAHH also used this as an opportunity to establish an Age-Friendly Regional Network for the Washington, D.C., metropolitan area. The CAHH partnered with GW Nashman Center, Georgetown University, and the age-friendly regional municipalities, and looks forward to building even more partnerships.
i. World Health Organization. (n.d.). Towards an Age-Friendly World. https://www.who.int/ageing/age-friendly-world/en/
ii. AARP. (n.d.). The 8 Domains of Livability: An Introduction. https://www.aarp.org/livable-communities/network-age-friendly-communities/info-2016/8-domains-of-livability-introduction.html
iii. Neal, M. & DeLaTorre, A. (2016), The Case for Age-Friendly Communities. Grant Makers in Aginghttps://www.giaging.org/documents/160302_Case_for_AFC.pdf
AUTHOR Meredith Lidard Kleeman





